The Book of Wisdom (PDF): A Comprehensive Guide
Discover the Wisdom of Solomon, readily available as a PDF, alongside Giguet’s 1872 French translation of the Septuagint. Explore this ancient text’s profound insights!
The Book of Wisdom, a significant text within the Deuterocanonical books, stands as a profound exploration of Wisdom itself – both as a philosophical pursuit and as a divine attribute. Often referred to as the Wisdom of Solomon, this work delves into themes of justice, righteousness, and the consequences of both virtue and vice. Its literary style is notably rhetorical and persuasive, aiming to guide readers towards a life lived in accordance with divine principles.
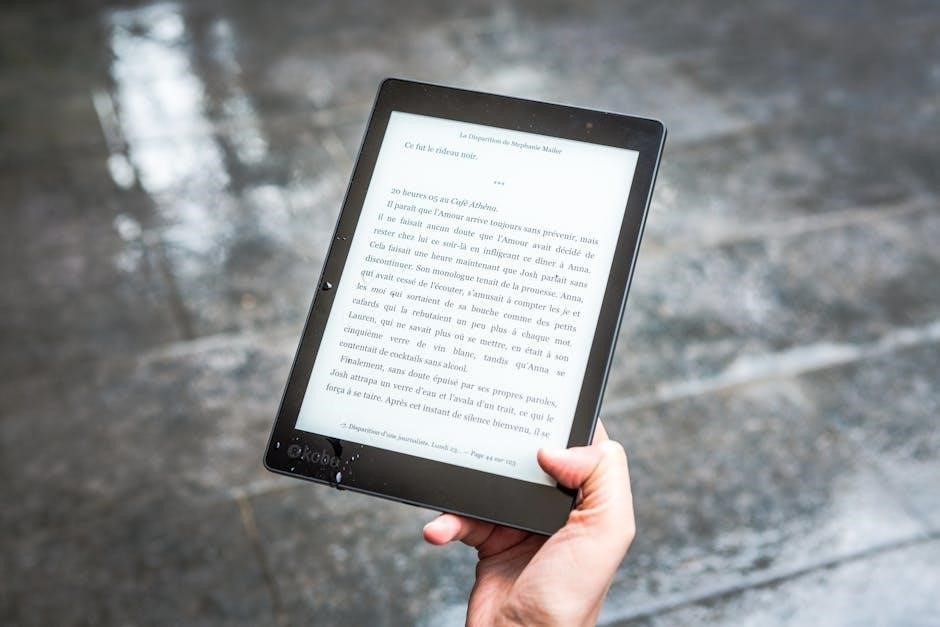
Access to this invaluable text is increasingly facilitated through readily available PDF versions, allowing for convenient study and reflection. These digital formats often include scholarly introductions and notes, enhancing understanding. The book’s enduring relevance stems from its timeless exploration of fundamental human questions concerning morality, purpose, and the nature of a fulfilling life. It’s a cornerstone for those seeking spiritual guidance and philosophical insight, offering a rich tapestry of thought for contemplation.

Historical Context of the Book of Wisdom
The Book of Wisdom emerged from a pivotal period in Jewish history, likely written during the Hellenistic era, specifically in Alexandria, Egypt. This context is crucial, as it explains the book’s engagement with Greek philosophical thought while firmly rooted in Jewish tradition. The flourishing Jewish community in Alexandria was exposed to Greek learning, influencing the book’s style and arguments. It reflects a time when Jewish scholars sought to articulate their faith in terms understandable to a wider, Hellenized audience.
Understanding this historical backdrop is vital when accessing the text today, particularly through PDF versions which often include contextual introductions. The book addresses issues of idolatry and injustice prevalent in the Hellenistic world, defending the Jewish faith against accusations of backwardness. It’s a testament to the intellectual and spiritual resilience of the Jewish community navigating a complex cultural landscape, offering a unique perspective on wisdom and divine providence.
Authorship and Dating
Determining the authorship of the Book of Wisdom remains a scholarly debate, traditionally attributed to Solomon, yet most scholars believe this is pseudepigraphical – written under Solomon’s name to lend authority. Internal evidence suggests a learned Jew from Alexandria, Egypt, composed the work, possessing a deep understanding of both Jewish scripture and Hellenistic philosophy. The author demonstrates familiarity with Greek literature and thought patterns.
Dating the book is similarly complex. Most scholars place its composition in the first century BCE, between 80 and 50 BCE, based on linguistic features and historical allusions. Accessing PDF versions of scholarly commentaries often provides detailed discussions of these dating arguments. The book’s focus on the folly of idolatry and the suffering of the righteous aligns with the historical experiences of Jews under Hellenistic rule, solidifying this timeframe. The text’s sophisticated Greek style further supports a first-century BCE date.
Original Language and Translation
The Book of Wisdom was originally written in Greek, unlike most other books of the Old Testament which were composed in Hebrew. This unique characteristic significantly impacts its interpretation and textual history. Accessing a PDF of the original Greek text allows for detailed linguistic analysis, revealing nuances often lost in translation.
Giguet’s 1872 French translation, based on the Septuagint, remains a valuable resource for scholars, readily available for download. The Septuagint itself is a Greek translation of the Hebrew Bible, predating the Christian era. Numerous English translations exist, each with its own strengths and weaknesses. When studying the text, comparing multiple translations – and ideally consulting the Greek original via PDF – is highly recommended. The quality of translation profoundly affects understanding of the book’s complex theological arguments and poetic style.

Content and Themes
Explore divine attributes, true wisdom’s nature, the perils of idolatry, and the concepts of justice and retribution within this insightful PDF text.
Wisdom as a Divine Attribute
The Book of Wisdom profoundly establishes wisdom not merely as human intellect, but as an emanation of God’s very being. This divine attribute is presented as intrinsic to creation itself, actively participating in the ordering and governance of the universe. The PDF version allows detailed study of passages illustrating wisdom’s pre-existence and role alongside God, particularly in shaping the cosmos and guiding righteous individuals.
It’s depicted as a radiant, all-pervading force, accessible to those who seek it diligently and live justly. The text contrasts this divine wisdom with the folly of idolatry, demonstrating how false gods are devoid of the power and understanding inherent in true wisdom. Studying the PDF reveals how the author emphasizes wisdom’s connection to immortality and its capacity to deliver from sin and death, solidifying its status as a fundamental aspect of God’s nature and a pathway to salvation.
The Nature of True Wisdom
The Book of Wisdom, accessible in PDF format, delineates true wisdom as far more than intellectual knowledge; it’s a moral and spiritual quality deeply rooted in a relationship with God. It’s characterized by righteousness, justice, and a profound understanding of divine order. The text emphasizes that wisdom isn’t acquired through worldly pursuits but through seeking God’s guidance and embracing virtuous living.
The PDF allows close examination of passages illustrating wisdom’s practical application – how it informs ethical conduct, fosters compassion, and leads to a fulfilling life. It’s presented as a discerning faculty, capable of distinguishing good from evil and guiding individuals toward sound judgment. Furthermore, the book highlights wisdom’s connection to understanding the universe’s purpose and recognizing God’s presence in all things, offering a holistic path to enlightenment and a life aligned with divine will.

Idolatry and its Consequences
The Book of Wisdom, readily available as a PDF, vehemently condemns idolatry, portraying it not merely as a religious error, but as profound folly and a grave offense against God. The text meticulously details how the worship of false idols stems from ignorance, a misconstrued understanding of the divine, and a descent into moral depravity. It argues that idols are lifeless creations, incapable of offering genuine help or protection.
Examining the PDF reveals a stark depiction of the consequences of idolatry: societal corruption, spiritual blindness, and ultimately, divine retribution. The book contrasts the true God – the source of all life and goodness – with the vain illusions offered by idols. It emphasizes that turning away from the true God leads to chaos and destruction, while embracing divine wisdom brings blessings and lasting peace. The text serves as a powerful warning against the seductive allure of false worship.
Justice and Retribution
The Book of Wisdom, accessible in PDF format, profoundly explores the themes of divine justice and retribution, asserting God’s unwavering commitment to righteousness. It meticulously examines the fate of both the righteous and the wicked, demonstrating that God does not overlook injustice but actively intervenes to ensure ultimate accountability. The PDF reveals a nuanced understanding of suffering, clarifying that it isn’t necessarily a sign of divine disfavor, but can serve as a test of faith or a consequence of past actions.

The text highlights that while the wicked may prosper temporarily, their triumph is illusory and ultimately leads to ruin. Conversely, the righteous, even in the face of persecution, will find solace and reward in God’s presence. Studying the PDF reveals that God’s justice isn’t merely punitive; it’s restorative, aiming to correct wrongdoing and establish a harmonious order. It’s a powerful testament to the enduring power of moral integrity.

Exploring the Text
Dive into the Wisdom of Solomon via accessible PDF versions, including Giguet’s 1872 French translation; discover key chapters and passages within this ancient scripture.
The Wisdom of Solomon and the Septuagint
The Book of Wisdom holds a significant place within the Septuagint, the ancient Greek translation of the Hebrew Bible. This translation, completed centuries before the Common Era, served as the scriptural foundation for many early Christians. Giguet’s meticulous 1872 French translation, based on the Septuagint, provides invaluable insight into the text’s nuances and historical context.
Accessing the Book of Wisdom as a PDF allows for detailed study and comparison with other ancient texts. The Septuagint version differs in some respects from the Masoretic Text, the standard Hebrew version, offering alternative interpretations and expanded passages. Scholars often utilize both versions to gain a more comprehensive understanding of the original meaning.
The Wisdom of Solomon, specifically, is considered deuterocanonical by Catholic and Orthodox Christians, meaning its authority is recognized, but not universally accepted by all denominations. The PDF format facilitates easy access to this important text for theological research, personal study, and comparative analysis of biblical translations.
Giguet’s French Translation (1872)
Emmanuel Giguet’s 1872 French translation of the Book of Wisdom, derived from the Septuagint, remains a valuable resource for scholars and enthusiasts alike. This translation is highly regarded for its accuracy and fidelity to the original Greek text, offering a nuanced understanding of the work’s literary style and theological depth.
The availability of this translation, often found as a PDF download, allows for convenient study and comparison with modern English versions. Giguet’s work provides a crucial link to the historical interpretation of the Book of Wisdom within a French-speaking theological tradition. It’s recommended for those seeking a deeper engagement with the text’s complexities.
Researchers appreciate Giguet’s detailed notes and annotations, which illuminate the cultural and historical context surrounding the Book of Wisdom. Accessing the PDF version enables easy searching and cross-referencing, making it an ideal tool for academic research and personal exploration of this ancient wisdom literature.
Availability of PDF Versions
PDF versions of the Book of Wisdom are widely accessible online, facilitating convenient study and dissemination of this ancient text. Numerous websites and digital libraries host downloadable copies, often including both the original Greek text (Septuagint) and various translations, including Giguet’s 1872 French rendition.
These PDFs cater to diverse needs, ranging from scholarly editions with extensive footnotes to simplified versions for personal reading. Searching online using keywords like “Book of Wisdom PDF,” “Wisdom of Solomon PDF,” or “Giguet translation PDF” yields numerous results.
Digital formats allow for easy portability and searching, making the text readily available on various devices. Furthermore, the proliferation of PDF versions promotes broader access to this important work of wisdom literature, fostering greater understanding and appreciation of its enduring message. Ensure sources are reputable for accurate content.
Key Chapters and Passages
The Book of Wisdom contains several pivotal chapters and passages that resonate with enduring theological and philosophical significance. Chapters 9-11, particularly, offer a profound meditation on wisdom’s origins and its relationship to God, detailing how wisdom was bestowed upon Solomon through prayer.
Passages detailing the condemnation of idolatry (like Chapter 13-15) powerfully contrast true worship with the futility of false gods. The narrative concerning the plagues inflicted upon Egypt (Chapters 16-19) serves as a testament to God’s justice and power over creation.
Scholars often highlight the exploration of justice and retribution throughout the book, particularly in its depiction of the fate of the righteous and the wicked. Examining these key sections within a PDF version allows for focused study and deeper engagement with the text’s core themes and literary artistry.

Related Concepts & Works
Explore connections between the Book of Wisdom, the Sibylline Oracles, Natalie Barney’s writings, and the concept of divine wisdom, all accessible via PDF.
Wisdom and Marie (Marian Connection)
Delving into the spiritual realm, the Book of Wisdom establishes a compelling link with Marie, representing a profound Marian connection. This association positions Marie as the house built by Wisdom itself, embodying the pinnacle of divine messengers sent to humanity. She is considered, in the highest degree, one of these virgin messengers, actively dispatched by Wisdom to guide and enlighten humankind.

This connection isn’t merely symbolic; it reflects a deeper theological understanding where Wisdom actively utilizes chosen vessels – like Marie – to manifest its presence and influence in the world. Studying the Book of Wisdom, often found in accessible PDF formats, reveals how this divine attribute seeks connection with humanity through figures of purity and grace. The text suggests that understanding Wisdom necessitates recognizing its embodiment in such sacred individuals, enriching our comprehension of both divine wisdom and Marian theology.
The Sibylline Oracles and Divine Wisdom
Exploring ancient texts alongside the Book of Wisdom, readily available as a PDF, reveals fascinating parallels with the Sibylline Oracles. These oracles were historically reputed as emanations of divine wisdom, offering prophetic insights and moral guidance. Both sources share a common thread: a belief in a higher power communicating with humanity through inspired individuals and texts.

The Sibylline Oracles, like the Book of Wisdom, often address themes of judgment, redemption, and the ultimate triumph of good over evil. Examining both in conjunction provides a richer understanding of the Hellenistic world’s spiritual landscape and the diverse ways divine wisdom was perceived and disseminated. Accessing the Book of Wisdom in PDF format allows for easy comparative study, highlighting shared motifs and unique perspectives on universal truths. This comparative analysis deepens appreciation for the enduring quest for wisdom across different traditions.
Natalie Barney’s “Pensées d’une Amazone” & Wisdom
Considering Natalie Barney’s “Pensées d’une Amazone” (1918) alongside the readily accessible Book of Wisdom PDF unveils intriguing connections to the pursuit of wisdom and unconventional thought. Barney’s work, a collection of aphorisms and reflections, embodies a fiercely independent spirit and a rejection of societal norms – qualities resonating with the Book of Wisdom’s call for discerning judgment and moral courage.
Both the Book of Wisdom and Barney’s “Pensées” challenge conventional understandings of truth and advocate for a personal, experiential approach to knowledge. While differing in form and context, both texts encourage readers to question established beliefs and cultivate inner wisdom. Studying the Book of Wisdom in PDF format alongside Barney’s work offers a unique lens through which to explore the intersection of ancient philosophical traditions and modern feminist thought, revealing enduring themes of self-discovery and intellectual liberation.

Practical Applications & Modern Relevance
Explore the Book of Wisdom’s PDF for spiritual guidance, connecting ancient wisdom to contemporary philosophy and refined expertise, like MSC Cruises’ “Art de la Croisière.”
Wisdom in Contemporary Philosophy
The Book of Wisdom, accessible in PDF format, offers a rich vein of thought for contemporary philosophical exploration. Its discourse on wisdom – not merely as knowledge, but as a divine attribute and a way of life – resonates with modern inquiries into ethics, virtue, and the meaning of existence. The text’s emphasis on discerning true wisdom from fleeting pleasures and worldly power provides a compelling counterpoint to consumerist and materialistic tendencies prevalent in modern society.
Philosophical investigations into the nature of wisdom often grapple with its subjective and objective dimensions. The Book of Wisdom presents a nuanced perspective, grounding wisdom in a transcendent source while simultaneously highlighting its practical implications for just governance and individual flourishing. Its exploration of justice and retribution, alongside the consequences of idolatry, invites critical reflection on societal structures and moral responsibility. Furthermore, the availability of Giguet’s French translation (1872) in PDF form allows for comparative textual analysis, enriching philosophical understanding.
The Book of Wisdom as a Source of Spiritual Guidance
The Book of Wisdom, conveniently found as a PDF, serves as a profound source of spiritual guidance, offering timeless wisdom applicable to contemporary life. Its exploration of divine attributes and the pursuit of true wisdom provides a framework for cultivating inner peace and moral integrity. The text’s emphasis on justice, retribution, and the consequences of straying from righteous paths encourages self-reflection and ethical conduct.
For those seeking spiritual nourishment, the Book of Wisdom presents a compelling vision of a life lived in harmony with divine principles. Its connection to Marie, viewed as a vessel of wisdom, and echoes within the Sibylline Oracles, deepen its spiritual resonance. Accessing the text via PDF, including Giguet’s 1872 French translation, allows for deeper engagement with its nuanced teachings. It offers solace, inspiration, and a pathway towards a more meaningful and purposeful existence, mirroring the refined expertise found in concepts like MSC Cruises’ “Art de la Croisière.”
Connecting Wisdom to MSC Cruises’ “Art de la Croisière” (Refined Expertise)
MSC Cruises’ “Art de la Croisière” embodies a refined expertise and meticulous attention to detail, mirroring the pursuit of wisdom detailed within the Book of Wisdom – readily accessible as a PDF. Just as the text champions discerning judgment and skillful living, MSC Cruises cultivates an experience defined by sophisticated service and curated journeys.
The Book of Wisdom’s emphasis on understanding the world’s intricacies resonates with the thoughtful planning behind MSC’s itineraries, from Mediterranean voyages to explorations of the Arabian Gulf and Norwegian fjords. Both represent a dedication to elevating experiences through knowledge and skillful execution. Exploring the PDF version of the text, alongside resources like Giguet’s translation, encourages a similar appreciation for nuanced understanding. Like the “Art de la Croisière,” the Book of Wisdom invites us to embrace a life of informed choices and refined appreciation.
“Les clés dor de Gaïa” ─ Elemental Wisdom Oracle (PDF Format)
“Les clés dor de Gaïa”, a 202-page elemental wisdom oracle available in PDF format (alongside ePub, MOBI, and other formats), parallels the ancient search for wisdom found within the Book of Wisdom itself. Both resources offer pathways to deeper understanding, though through different modalities. While the Book of Wisdom, accessible as a PDF, presents philosophical and theological insights, “Les clés dor de Gaïa” utilizes elemental archetypes for intuitive guidance.
Julia Skorupska’s oracle, ISBN 9782381354262, provides a contemporary lens through which to explore timeless wisdom themes. Like studying Giguet’s 1872 French translation of the Book of Wisdom, engaging with this oracle requires a willingness to contemplate symbolic language and inner knowing. Both resources, in their distinct ways, encourage self-reflection and a connection to something larger than oneself, offering tools for navigating life’s complexities.





















































































Leave a Comment